The right service changes at the right time: empowering nurses to lead amid COVID-19

The initiatives that show collective leadership is not about targets but staff working together

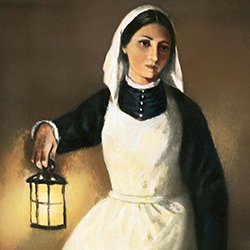
In April 2019, I started a year-long leadership scholarship for aspiring nurse directors with the Florence Nightingale Foundation.
This involved undertaking a patient care improvement project, and my initial focus was on quality improvement in a Northern Irish context.
Change takes time – except during a pandemic
Over the past few years, the six health and social care trusts across Northern Ireland have been striving to deliver quality improvement through service and staff development programmes, aiming to make this part of their culture.
Although you may expect transformation to happen quickly in a relatively small region such as Northern Ireland, change can take a long time. This is due to many factors, including financial restraint, bureaucracy, and the sometimes complex relationships between different organisations, professionals, patients and carers.
When the COVID -19 pandemic emerged in Europe, however, it changed the face of healthcare as we know it.
Staff had to respond rapidly to a dynamic and challenging environment, and when it came to writing up my project, my work looked dated compared to the improvements happening due to COVID-19.
What is collective leadership?
The collective leadership strategy is a relatively new approach to leadership in Northern Ireland. It aims to move away from imposing top-down solutions and recognises that front-line teams, service users and carers are best placed to explore important issues and identify solutions.
Centralised health and care structures hinder innovation and dampen staff morale
Along with the rest of the UK, services in Northern Ireland had to be re-profiled to prepare for the pandemic, and measures put in place quickly to deal with the predicted surge in patient numbers.
At Belfast Health and Social Care Trust, a COVID-19 oversight group was formed. As a nursing and midwifery leader, I am part of this group, along with senior staff from across the trust who are responsible for providing leadership and empowering staff to mobilise change.
‘When initiatives come from staff, they have a sense of purpose, energy and enthusiasm and are more likely to succeed’
As leaders, the group were aware that staff engagement is an essential component of quality improvement; a review of reform in Northern Ireland carried out by The Nuffield Trust, published in July 2019, found that the centralised nature of health and care structures was dampening down innovation.
As well as creating a lack of pace around change and improvement in the region, this could have a negative influence on staff morale and empowerment, the report said.
We knew that if we focused on pushing ahead with initiatives without acknowledging how teams were feeling, we could potentially lose their trust. This could result in staff becoming disengaged, which would be detrimental to success.
View our COVID-19 resource centre
Harnessing the experience of front-line teams, carers and service users
When initiatives come from staff, they have a sense of purpose, energy and enthusiasm and are more likely to succeed.
Through joint working, teams across the trust quickly identified opportunities for rapid improvement and learning within current practice, and I witnessed first-hand the benefits brought about by staff empowerment and collective leadership.
The oversight group held twice-weekly team meetings via teleconference with senior representatives from multidisciplinary teams, who were in a position to understand what was required for their area and could drive change.
Finding ways to improve care and communication during the COVID-19 outbreak
Collective leadership requires us to develop shared leadership within teams, based on supportive communication and mutual feedback. One of the most important features of these team meetings was that they were a safe space for staff to share their thoughts and concerns openly and honestly, and to make suggestions for improving patient care.
The group also worked closely with staff deployed to the COVID-19 testing pods. Recruiting to this team was initially challenging as staff were anxious about the personal risk of being exposed to the virus. A collective leadership approach was paramount for staff who had stepped forward to run this service, with the team encouraged to make any changes required to the testing pods and processes to ensure the service was responsive and effective.
Staff-led changes to improve care
Although no financial constraints were imposed on teams, the changes made were not about money, they were about new ways of working.
The initiatives that teams were able to implement quickly included:
- Using technology to assess and support patients.
- Improving patient flow to ensure patients attending the emergency department (ED) were seen quickly and moved to the right ward or discipline as soon as possible.
- Using staff in different ways, including redeploying staff from downturned services such as outpatients to the ED, to help expedite decisions to admit, and deploying staff to hospital wards to support ward staff in discharging medically fit patients.
- Supporting more patients at home to prevent hospital admissions.
While the team communicated any issues to the oversight group, they also often had suggestions to ameliorate problems, such as establishing better connections to other services across the trust, including laboratories and occupational health services.
With visitor restrictions imposed during lockdown, the trust’s call handlers became increasingly overwhelmed with calls from families. A number of complaints were received from families who had not been able to get through to ward telephones, so had not received updates about their relatives.
After being asked by the oversight group to consider how they could reassure families, the patient experience team quickly set up a patient liaison service, using staff from the redeployment list from a range of disciplines across the trust.
Leadership through support: what I learned from the programme
The COVID-19 preparations and changes to practice were driven by empowered staff.
Change was not about performance or targets but about working together as a collective for the best outcomes for patients – exactly what quality improvement is all about.
Florence Nightingale was a champion of improvement, specifically improvements designed to reduce patient suffering and improve compassionate, patient-centred care. Her drive to improve set the standard for the continuous improvement today’s nurses and midwives aspire to achieve, and I am proud to be a Florence Nightingale scholar in the year we celebrate the bicentenary of her birth.
Undertaking the scholarship programme helped to prepare me for this leadership challenge, and my learning from the programme has been vital during the pandemic. By understanding myself better, I was able to challenge my thinking about how I support and empower nurses and midwives.
The programme also gave me the confidence to lead others and inspire them to drive improvements to patient care, encouraging them to be flexible and responsive at this challenging time.
A lot has been achieved in a short time
The COVID-19 pandemic has been – and still is – a frightening time for many people. Florence Nightingale said how ‘little can be achieved in the spirit of fear’, yet through courageous leadership and supporting and empowering staff, so much has been achieved in a short space of time.
It is difficult to see how there would be an appetite to return to how we did things before COVID -19, where strategic transformation was centralised, front-line staff felt removed from improvement initiatives and change took so long to deliver.
The focus for healthcare leaders now will be to capture the learning from the pandemic and understand how we use this to continually improve the way we work.
 Brona Shaw is deputy director of nursing at Belfast Health and Social Care Trust in Northern Ireland
Brona Shaw is deputy director of nursing at Belfast Health and Social Care Trust in Northern Ireland
Further information
Florence Nightingale Foundation: Leadership Scholarship 2020
