Barriers to maintaining continence
It is estimated that more than three million people in the UK are affected by incontinence which has no anatomical cause. The person may be rendered incontinent because of physical, psychological, emotional, cognitive or environmental factors. Some of these are listed below.
Learning/cognitive disability
Learning disability or cognitive impairment needs to be taken into consideration when carrying out a continence assessment. Bowel and bladder control may take longer to develop in individuals with learning disabilities. Specialist continence support for these people can result in them becoming continent.
Language barrier
We must make sure, wherever practical, that arrangements are made to meet patients’ language and communication needs.
Mobility
If a person has the ability to know when they need to go to the toilet, but are unable to do so independently, they may experience continence issues.
For some people, accessing the toilet can be so challenging that using a pad or requesting a catheter is easier than trying to remain continent. If the person is a wheelchair user and needs support to go to the toilet, it can be particularly challenging as help is not always available in a timely manner.
A full assessment may identify toileting aids and equipment (such as urinals, handrails, commodes and removable clothing) that can support an individual to remain independent and, in some cases, major adaptations such as hoists, downstairs toilet or stairlift may be appropriate.
Environmental factors
When people are out and about in the community, toilets can often become an issue. The location and accessibility of toilets can be a barrier to continence, and with councils closing more public toilets it makes getting to a toilet even more difficult.
In general people do not like to be heard on the toilet or may be embarrassed when using public toilets. Often these facilities are not clean and can be unpleasant to visit. If a person does not have a choice in where they go to the toilet, it may become preferable to be incontinent than use an unsuitable bathroom or toilet.
People with Autistic Spectrum Disorders (ASD) may only be able to use a toilet in the home environment or use certain toilets when they are in an unfamiliar place, so this will need to be planned before going outside of the home.
Flooring in bathroom areas need careful consideration as certain colours or shiny floors can make the floor look wet and cause problems for people with visual impairments.
Care homes and hospitals often locate toilets away from main areas and they may be poorly marked or signposted. If an individual cannot locate the toilet or it is too far away, involuntary incontinence may occur.
Often signage on toilet doors can be confusing, especially for people with dementia. Complicated or modern icons might be used, which some people may find difficult to recognise as the place where they can go to the toilet.
Other examples of where the environment can make it difficult for people to go to the toilet:
- poor maintenance of public toilet facilities – wet, dirty floors
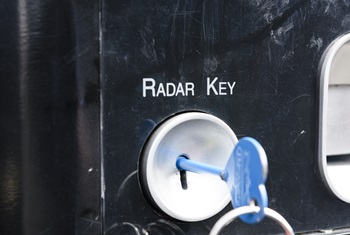
- many accessible facilities need a Radar key to gain access, which can be obtained from the local council
- poor consideration of space needed by wheelchair users or people with young children in pushchairs
- doors are often heavy and open outwards, requiring assistance from another person to gain access
- no hoists or changing plinths in the majority of accessible facilities
- person has to transfer to the toilet by standing or using transfer aids
- a limited number of cubicles in men’s toilets and lots crammed into ladies toilets, making it hard to gain privacy if they have diarrhoea or offensive smelling stools or flatulence.
Assessing an individual for the correct equipment to manage and maintain their continence is imperative. It will require input from a specialist continence professional who may be a nurse or an occupational therapist.
There is a wide variety of equipment on the market and finding the most appropriate for the individual is vital. The types of equipment may range from raised toilet seats to highly specialised toilets that may include the facility to wash the person.
Simple things that can help support people with incontinence include:
- toilet paper is always available
- the bathroom area is clean
- toilet doors are able to close
- sufficient space and access needs to be provided to allow for staff, wheelchairs and other aids.
Clothing
Clothing can be a barrier to managing incontinence. If a person has poor manual dexterity, they can find it difficult to undo or pull-down garments. There are a number of companies which manufacture clothing that is easy to remove, pull down, etc. For example, skirts with velcro sides, trousers/pants with drop down fronts. These garments look functional and unfashionable or just unappealing and people should seek advice about where they might find clothing that meets their needs and looks nice. As an alternative, it may be possible to alter existing clothing to make dressing and living with incontinence more manageable.
Equipment and devices
A number of products are available to help with the management of incontinence. These include:
- handheld urinals (urine collection bottles)
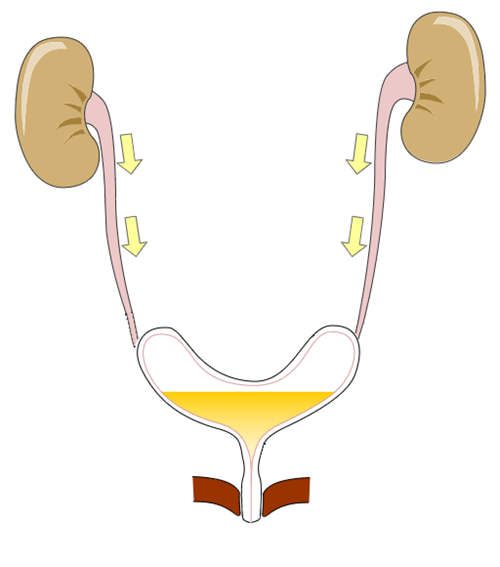
- a catheter, a thin tube that is inserted into the bladder to drain urine. It may be used intermittently or on a long-term basis
- devices that are placed into the vagina or urethra to prevent urine leakage, for example during exercise
- urinary sheath
- absorbent products, such as incontinence pants or pads.
Urinary catheters
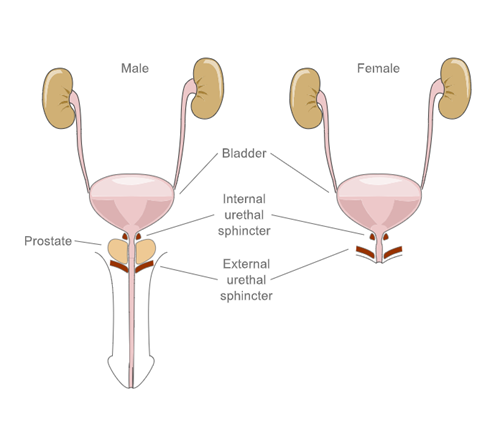
Following your clinical assessment and collaborative decision making on the need for a urinary catheter consideration then needs to be given on make (potentially guided by local formulary), size (sex, urethral/ suprapubic and clinical assessment) and type:
Indwelling (Short term) – used for 28 days or less
Indwelling (Long term) – used for up to 12 weeks
Intermittent - inserted several times a day, for just long enough to drain the bladder, and then removed
A Suprapubic (SP) Catheter is initially surgically inserted through the skin to the bladder, it is important to check that the catheter is licenced to be used for a SP Catheter.
Further resources
RCN (2019) Catheter care: guidance for health care professionals
NHS England. Urinary catheter tools
NHS (2020)Types of urinary catheters
Toilet Aides
Bed pans
Bed pans are a portable receptacle for bed bound patients. They are often made from a plastic which can be washed at high temperatures or recycled or moulded pulp that can be disposed of after use.
Positives: low cost, can be reusable and easy to clean.
Negatives: User may find it uncomfortable to use while lying down. User may need assistance to get bed pan in position.
Commodes
Commodes are a chair with concealed toilet bowls. Commodes are available with the following features designed to make them comfortable, convenient and stable, such as adjustable height, removable arms, splayed legs and footrests.
Positives: Discreet, can be placed near the bed for easy access at night, some are suitable to be used as shower chairs or can be wheeled over a normal toilet.
Negatives: The commode and pale require regular and thorough cleaning and disinfection to prevent cross infection.

Free-standing toilet frame
A free-standing toilet frame is made from a steel frame that locates around the toilet to offer toileting support. A Sani chair is similar but with a toilet seat attached.
Positives: flexible can be altered to be the correct height for the patient. No need for building alterations.
Negatives: not secured to the wall or floor – could tip or cause entrapment.

Floor / wall mounted toilet supports
Floor / wall mounted toilet supports are useful where space is limited as they can be folded up out of the way when not required. They are particularly appropriate for users who may be transferring to and from a wheelchair.

Raised toilet seat
The raised toilet seat can be fitted over the existing toilet seat and is secured in place to the toilet bowl with two clamps at the rear, available with or without lid.
Positives: Easy to fit, available in different heights depending on patient.
Negatives: risk of falls if not fitted correctly.


RADAR keys
RADAR keys: The Royal Association for Disability and Rehabilitation, which is now Disability Rights UK, worked in partnership with Nicholls & Clarke, the inventors of the RADAR lock and together they created the National Key Scheme (NKS). The first RADAR locks were fitted in 1981 to help keep accessible toilets free and clean for disabled people.
Positives: Easily available from most local authorities who will sell or give a RADAR key.
Negatives: If you are travelling to Europe, the RADAR key will not work so you will need to buy a Euro key
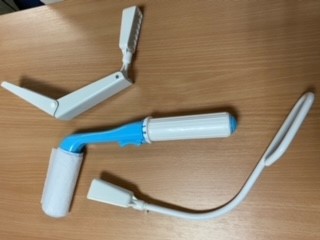
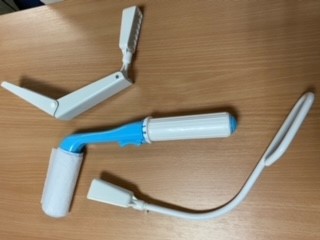
Bottom wipers
Bottom Wipers are designed to help those who may have limited dexterity or other mobility issues with their personal toilet hygiene, it is a discreet and effective, it is a bathroom aid that can help maintain personal hygiene when reaching becomes difficult.
Positives: promotes independence reducing cost of carers. Maintains skin integrity by preventing body fluids to damage the skin.
Negatives: Unable to see if bottom is clean and condition of skin.
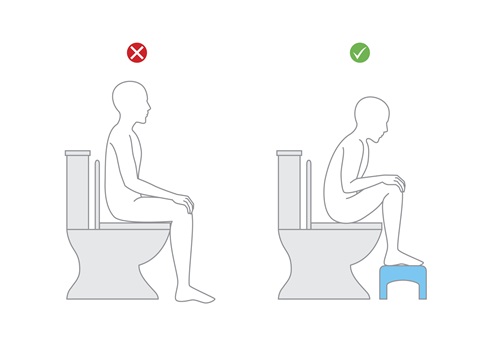
Foot stools
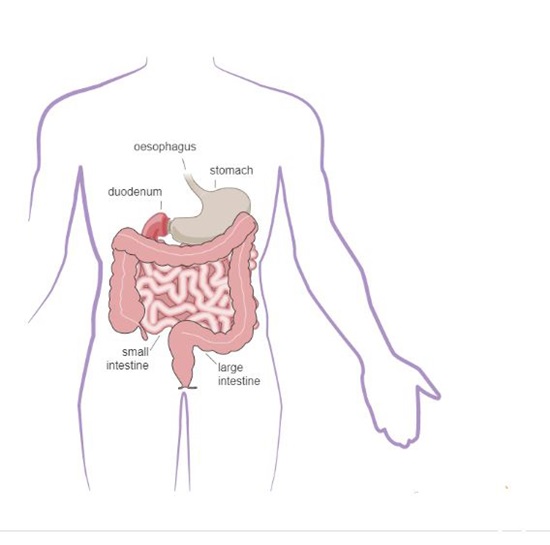
Foot stool are to assist in achieving the 'right' angle when going to the toilet. When squatting, the puborectalis muscle loosens creating a straight passageway into the rectum.
Positives: easy and discreet storage when not in use.
Negatives: risk of falls if person forgets that their feet are raised off the floor.

Body suit
Body suit is made in the UK from 100% cotton, which provides the user with exceptional comfort. Cotton bodysuits are the ideal solution to provide extra security for keeping incontinence pads in place whilst also helping to prevent tapes from coming unstuck. The bodysuit features 3 metal steel snaps at the crotch to allow for easy access and fitting. For maximum hygiene, the cotton bodysuit can be either machine or hand washed up to 40 degrees Celsius
Positives: added security for those worried that incontinence pads may become dislodged or at risk of choking from Superabsorbent Polymer in pads.
Negatives: Risk assessment may be required if used in patients’ best interest.

Male Continence devices
Male devices are a range of products that men can use as alternatives to absorbent pads. They are divided into two main categories according to their function:
Some are designed to contain bladder leakage this includes sheaths and body-worn urinals.
Some are designed to prevent bladder leakage – such as the penile compression device or clamp.
Portable urinals for men
These are designed specifically to fit the male anatomy and to be convenient to the user.
Positives: Male urinals can be put into position by or for the patient as and when required. Some have an option to add a drainage bag.
Negatives: Urinals can be heavy to manage when full and a patient’s hand control is poor, they may need assistance to empty the urinal. Risk of spillage if the patient.

Sheath
Is very similar to a contraceptive condom. It fits over the penis and collects urine as it leaves the body. You may also hear them called Condom catheters and will be connected to a leg drainage bag or a night drainage bag.
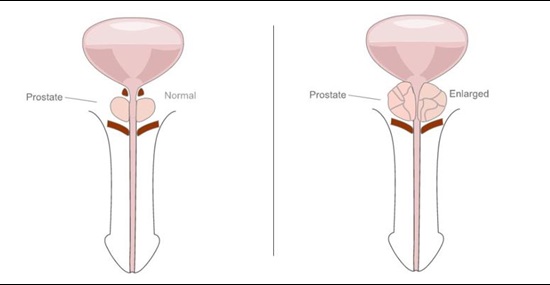
Positives: Sheaths are supplied in a range of lengths and sizes. Ensure a size that provides a secure fit without being too tight. If the man has a shortened penis (this is common after some treatments for prostate cancer) there are sheaths available in shorter sizes with the adhesive band nearer the tip of the sheath and extra thin sheaths.
Negatives: They don’t work well if the man has a short or retracted penis and in which case products designed specifically for this purpose may work better.

Devices for penile retraction
Pubic pressure urinal
This is a reusable product made out of latex, it consists of a ring which is held in place with straps or underwear in the same way as body-worn urinals but the ring is held firmly in place against the pubis and applies pressure to help the penis to protrude.
Positives: Pubic-pressure devices are effective in men with a retracted penis. They are available as single devices or integrated in underwear
Negatives: they require specialist assessment for the correct size and fit, as when the fitting is incorrect, these devices can cause tissue damage.
Male external continence device
This is an innovative external continence device which enables men to manage their own urine output with confidence. It offers an effective longer lasting alternative to sheaths and pads and can be used for up to 48 hours.
Positives: Good for men with a retracted or shorter penis. Longer wear time than standard sheaths up to 72 hours.
Negatives: When first using the device the device, the body will need to get used to the hydrocolloid in the adhesive. This phase normally takes 24-72 hours after the first application depending on the condition of the skin (this is not always visible). During this period the device the device, may need to be replaced more often, whilst the hydrocolloid absorbs any excess moisture.
Penile pouches / Male urinary pouch external collection device
These are small urine collection bags with an adhesive ring that is stuck onto the pubic bone around the penis. The hole can be cut to size to fit different penis widths.
The pouch collects urine and there is a tap at the bottom to allow the user to empty it into a toilet or urinal.
Positives: They are usually disposable and can be worn for 24-48 hours.
Negatives: it may be necessary to shave or trim the pubic hair in order to ensure that the adhesive can hold the pouch in place properly. It is likely that they work better in a standing position rather than seated.

Female continence devices
Portable urinals for women
These are designed specifically to fit the female anatomy and to be convenient to the user.
Positives: Most female urinals have a flat narrow end which can be easily put into position underneath the patient. This can be particularly useful if the lady is not very flexible and has difficulty moving her legs apart.
Negatives: Urinals can be heavy to manage when full and a patient’s hand control is poor, they may need assistance to empty the urinal. Risk of spillage if the patient has to lie down.

Funnel
A funnel is designed for women to use out of bed. It is recommended that the woman sits on the edge of a chair/bed or stands and holds the funnel in place.
Positive: The funnel is moulded from a soft plastic, which comfortably seals with the skin and helps minimise leakage.
Negatives: must be used with a drainage bag, leg bag or bottle bag.

Female hydrophilic urine director
Allows a woman to pass urine while standing or in a wheelchair.